Natural Biofilm Disruption
One of the most common topics people want to discuss with me is how to treat chronic infections. If this sounds like you, know that you are not alone! According to the National Health Council, generally incurable and ongoing chronic diseases affect approximately 133 million Americans, representing more than 40% of the total population of this country. However, to understand how we can fight such infections, we must first understand what a biofilm is.
These diseases include many conditions, including ones caused by bacteria. Such infections might include chronic Lyme, sinusitis, prostatitis, urinary tract infections, ulcers, bacterial vaginosis, vaginitis, lupus, periodontal disease, pneumonia, otitis, implant & catheter-related infections, and even chronic wounds (and too many more to list here). Today I’m going to focus on bacterial infections specifically because there is something you can start doing right away to help in that fight.
Antibiotics Are Sometimes Ineffective
Why are so many chronic conditions refractory to multiple antibiotics in otherwise healthy individuals? When antibiotics fail, we often put the blame on bacterial resistance. NOT SO FAST! This isn’t always the case. The antibiotics would often work fine if they could reach the bacteria. Unfortunately, and in many cases, the bacteria have not only figured out a way to avoid our immune system, but they have also figured out a way to protect themselves from the medications we have introduced them to.
The Stealth Infection
Many of these chronic infections are now considered “stealth infections” because they are hard to discover using conventional testing methods – meaning that they are both hard to diagnose and hard to treat. The symptoms and inflammation are there, but cultures will often show a “negative” result. This can be frustrating for both you and your doctors.
Logically, the mechanism that inhibits the antibiotics from working is the very same mechanism that hides their presence from standard cultures. Unfortunately, and in more cases than you would like to know, antibiotics worsen the problem. In a cruel twist, this makes it even more difficult for our immune system to locate and fight them because while the body recognizes something wrong, it can’t isolate the problem effectively enough to do anything about it.
So what is the mechanism, and what can we do?
Biofilms Are REAL
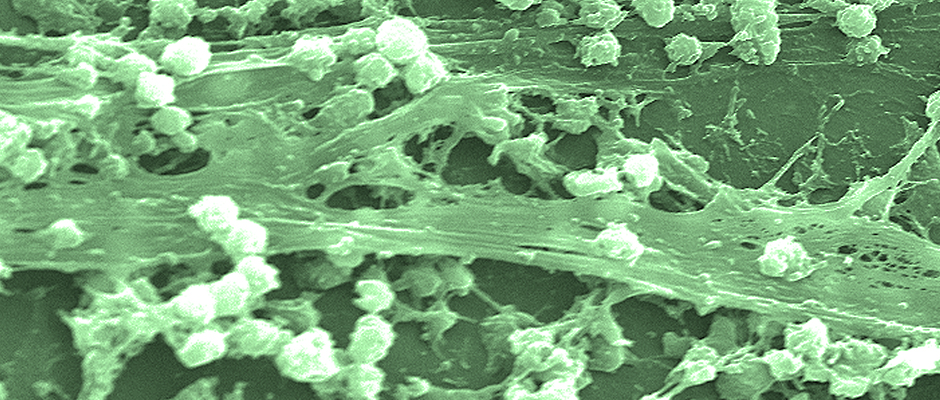
Chronic bacterial infections that the body can’t effectively fight are hard to test for and seemingly untouched by antibiotics. These chronic bacterial infections are often caused by bacteria growing in slime-enclosed aggregates known as biofilms. Of course, that’s probably not the best name for them, considering their true makeup, but the name helps keep everyone on the same page. Regardless, biofilms are implicated in many chronic infections and affect millions yearly. In fact, according to the NIH, more than 80% of human bacterial infections are associated with biofilms. Some studies have shown that antibiotics may help produce biofilms or worsen existing ones. Sadly, many deaths occur due to the immune system further eroding.
A somewhat technical way to describe a biofilm is bacteria that hide out in polysaccharide matrices created by the microorganisms. Sometimes they are even comprised of the “bio-junk” left behind by viruses or other bugs. Essentially, the bacteria have placed themselves into a nearly impregnable layer of slime that resists penetration by either antibiotics or even your natural defenses. The result may be infections that are not only difficult to treat but can also be deadly in the long run.
This is not to say that such bacteria cannot be found or even treated. In fact, these bacteria can usually be found quite easily when tissue biopsies and DNA tests are performed. However, many doctors are not going to venture such steps for conditions that are not killing you “right now” or for conditions that are hard to distinguish from other ailments.
Why Is This Happening?
That is a great question. Unfortunately, there is not an “easy” answer to this. Some blame biofilms on antibiotics, some blame it on a weakened immune system, and some blame it on the constant poisons we pick up from our environment. I don’t see the difference because the result is the same and because one directly impacts the other. For instance, if we blame a compromised immune function, then we need to ask ourselves why so many have compromised immune function in the first place. Of course, antibiotics and poisons are a good place to start. Now we’ve come full circle and need to break the cycle.
To break this cycle, you must start by reviewing your part in things like too many antibiotics, poor sleep, and bad food choices. Then you need to factor in things like chronic stress, poor lifestyle choices (like excessive drinking or drugs), isolation, and insufficient exercise. A combination of any of these could be a disaster waiting to happen. You could also take a look at your environment. Examine the flame retardants around you, chemical residues, and so on. Everything you eat or come into contact with will undoubtedly play a role.
The good news is that simply changing or avoiding even a few (or all) of these factors can help you prevent infection or help your body set the stage for recovery. It doesn’t have to be over-the-top, though. Just make minor adjustments.
Of course, if you’re already infected, setting the stage for recovery is only part of the battle. We also need to address the infection and the biofilms that protect them. This can be difficult and can take some time.
So What Can Be Done About Biofilms?
A few things can be done, but it depends on which routes you are willing to take. Every situation is different, and it will likely depend on how good of a doctor you are working with. Still, your doctor might try draining identified abscesses (if any are found) or trying high doses of antibiotics known to penetrate biofilms. Of course, these options may not be the best for you, but they are nonetheless options to be aware of. Thankfully, there is still another option.
The Natural Way
Researchers have been proactively searching for agents that disrupt and dissolve biofilms ever since they realized biofilms were a thing. In that quest, they stumbled upon a few great options, and new ones are being found daily. Fortunately, many of them are available to you now and over the counter.
But do they work? The answer is yes! It has even been demonstrated that biofilm disruptors can help mainstream antibiotics work better. And as it turns out, even natural antibiotics may be quite effective when used with natural biofilm disruptors. Of course, we are also discovering that biofilm disruptors taken by themselves can yield amazing results because the immune system alone is quite powerful when it has the right tools. This is also an essential point regarding prevention as well. Implementing what I’m about to share into your diet could help keep nasty infections from ever taking root.
Thankfully, nature (and science) has provided us with several biofilm disruptor options that also serve other beneficial functions in the body. This doesn’t happen overnight, though. Remember that chronic infections have had time to set up their defenses. You’re likely in for a fight. However, taken over a long enough period (times vary), many people can see improvement or even complete resolution of their chronic conditions.
Let’s start with my favorites – links for product suggestions have been provided and can be viewed by clicking on the suggestion title.
- Carvacrol: Found in Oregano oil, carvacrol has a long list of documented benefits for the body. Not only has it been found to inhibit antibiotic-resistant bacteria, viruses, parasites, and fungi, but it has also been shown to have high antibiofilm and antivirulence activities against certain species. I’m listing this specifically due to its diversity of benefits and overall effectiveness. However, due to its potency, you may want to ease into it and take it over an extended period of time, along with other biofilm disruptors.
- N-acetyl-L-cysteine (NAC): NAC is an amino acid derivative that is well-known in the medical community. In fact, I have listed it in other articles on this site because of the amazing things that it can do regarding many different conditions. It is listed here because not only can it be a useful therapy for autoimmune/inflammatory diseases, but it helps to boost glutathione production (which a well-functioning immune system is highly dependent on) AND BEST OF ALL… it is recognized as a “powerful molecule” against biofilms in numerous different infections.
- Proteolytic enzymes: Proteolytic enzymes create the dissolution of fibrin in the body and can help to destroy certain biofilms. In fact, enzymes such as nattokinase and lumbrokinase have been used extensively as coatings on implants to fight biofilms and have even been used successfully in the battle against Lyme. Highly fibrinolytic enzymes such as Serrapeptase, Lumbrokinase, and Nattokinase have all been said to help in various conditions, but you may need to try each to discover which one is most effective for your particular condition. I usually recommend that people try lumbrokinase first because it has also been used to help deliver medications deep in the body, it helps prevent and break up blood clots, and it is an amazing biofilm fighter.
Other Great Natural Options or Additions
While the previous options are great, that doesn’t mean that they will necessarily be perfect for your situation or even all that you need. Some conditions require specific options, slower eradication rates, or even more firepower. The following may not be as effective as the previously listed options by themselves, but they are worthy of mention due to their effectiveness in certain situations. More research may be needed on your part.
The first thing I should probably share in this regard surrounds the idea of Defensins. Defensins are antimicrobial peptides exhibiting antibacterial, antifungal, and antiviral activity. When it comes to bacterial infections, Defensins have broad-spectrum activity against both gram-positive and gram-negative bacteria. In the intestine, AMPs are produced and secreted by epithelial cells to help protect us against pathogens. Interestingly enough, stimulating epithelial cells to create the AMPs can be done with a combination of andrographolide (Andrographis) and isoliquiritigenin (a compound found in licorice)(STUDY).
With that being said, we should turn to some old favorites.
- Garlic &/OR Garlic Extract: Garlic and Garlic extracts have been shown to inhibit biofilm structures and have been used for many years as natural antibiotics. However, the concentration of garlic seems to have a direct relationship with the inhibitory effect. This means that you will likely need to take it more than once a day and over an extended period of time and/or include it with other agents for a more powerful effect. This could be a problem for some because garlic gets its odor from something called “allicin.” Something else to mention is that allicin is often attributed to the biofilm disruption capability, so odorless garlic simply may not be strong enough because the allicin content has been reduced. Still, this is a powerful tool for those who don’t mind that delicious garlic smell or wish to avoid “the herx“.
- Monolaurin: Created from coconut oil, this powerful supplement may help inhibit the development of biofilms in some species. Note that this likely means that the potential benefits are bacterial strain-specific, and it may not work well for all conditions. However, it may provide an added kick with the previously listed recommendations if you are looking for a boost. If not, it could be something to try if you’ve tried everything else or if you are eager to explore its other antibacterial or immune-boosting benefits. Lauric acid, Lauricidin, and related products might also work.
- Curcumin: Found in turmeric, curcumin is known to possess antimicrobial, analgesic, anti-inflammatory, and anticancer properties. On top of the anti-pathogen benefits, curcumin has also been deemed significantly effective at disrupting biofilm when taken along with certain antibiotics. Like monolaurin, it may be something to try in tandem with the previous recommendations or with your current antibiotic therapies. Just be sure to talk to your doctor before taking it with your medications.
Good luck, and keep up the fight! I will add to this list as more options are discovered. In the interim, be sure to check my article titled “The N-acetyl Cysteine (NAC) Powerhouse.” It covers the strong biofilm fighter discussed in this article more in-depth.
Dr. Robertson is a health researcher and educator, not a physician. The information provided here is not medical advice, a professional diagnosis, opinion, treatment, or service to you or any other individual. The information provided is for educational and anecdotal purposes and is not a substitute for medical or professional care. You should not use the information in place of a visit, call consultation, or the advice of your physician or other healthcare providers. Dr. Robertson is not liable or responsible for any advice, course of treatment, diagnosis, or additional information, services, or product you obtain or utilize. IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY, YOU SHOULD IMMEDIATELY CALL 911 OR YOUR PHYSICIAN.